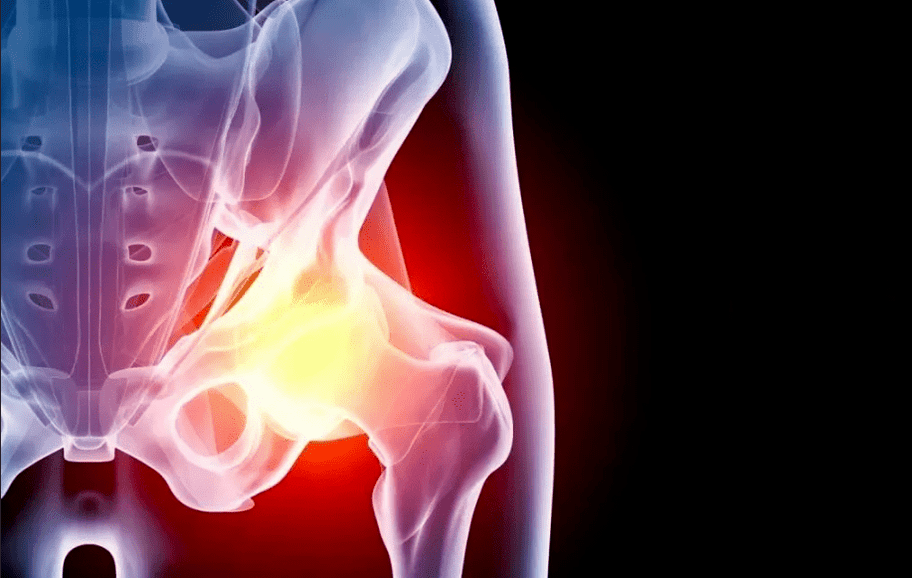
Hip arthropathy (hip arthropathy) is a chronic pathology, accompanied by the gradual destruction of cartilage tissue in the affected area, and subsequent involvement of adjacent structures in the process. This disease requires long-term treatment. In severe cases, the only way to restore mobility is joint replacement.
General information
Hip joint disease is a degenerative disease. It starts with microscopic changes in cartilage structure. Increased pressure, inflammatory diseases, and blood supply disorders cause structural transformation and thinning of cartilage tissue, which in turn deforms the contours of the joint area. As a result, the load distribution on the bone contact surface changes, and the areas with the greatest pressure begin to wear faster. This triggered a series of pathological reactions:
- Microcracks and compacted areas appear in cartilage tissue;
- The smoothness of the articular surface is reduced;
- Cartilage overgrows in the thinned area and is replaced by bone tissue;
- Osteophytes (bone growth) appear along the edges of joints;
- Thickened joint capsule and decreased elasticity;
- Hardening of ligaments and reduced strength;
- Changes in the composition of synovial fluid (natural lubrication in the joints);
- Narrowing of the joint space;
- Fusion of all elements of the joint (stiffness).
If left untreated, hip joint disease will inevitably become a cause of inconvenience and disability.
reason
According to the reasons for the development of the disease, primary and secondary hip joint diseases can be distinguished. In the first case, it happens on its own, for example, in the context of genetic predisposition, in the second case, it is caused by other diseases or injuries. In most cases, the degradation process of cartilage tissue occurs due to the combined action of a variety of factors. reasons may be:
- Congenital dislocation of the hip;
- Flat feet, scoliosis and other orthopedic problems;
- Legg-Calve-Perthes disease;
- Joint inflammation (arthritis), regardless of origin;
- Hip joint injuries and microtraumas under the background of overweight, professional sports, etc. ;
- Hip dysplasia;
- Metabolic disorders;
- Endocrine diseases (especially diabetes);
- Violation of the blood supply of the lower limbs;
- Frequent stress
- Genetic (hip joint disease of parents or other close relatives significantly increases the risk of hip joint disease in children);
- Congenital diseases and connective tissue autoimmune diseases (joint hypermobility, rheumatoid arthritis, systemic lupus erythematosus, etc. );
- A joint operation was carried out.
Age is an important predisposing factor. According to statistics, 45 years later, the possibility of hip joint disease has increased significantly.
symptom
The main symptoms of hip joint hip joint disease do not depend on the cause of the development. Most patients pay attention to:
- Movement limitation: One of the earliest symptoms caused by the thinning of the cartilage layer and increased friction on the bone articular surface; in the future, the appearance of cartilage hyperplasia will further aggravate this problem;
- Pain: The bones that have lost the cartilage layer rub against each other, all the elements of the joint are gradually involved in the degenerative process, and the reduced blood supply to the tissue causes the pain to increase as the disease progresses; the pain is intense in nature and usually worsens at the end of the day;
- Muscle spasms, which lead to aggravation of pain symptoms and limited joint range of motion;
- Decrease in leg length: This symptom appears in the later stages of the disease. This is due to the narrowing of the joint space and the gradual grinding of the bones of the head due to constant friction; the difference between the legs can reach 2 cm;
- Limp: related to severe pain and movement limitation and leg shortening; it is an unfavorable sign that the joint device is severely damaged.
stage
In the development process, hip joint disease goes through several stages, depending on the degree of tissue damage.
- 1 degree. At this time, the patient noticed that the joint pain that appeared after strenuous or prolonged physical activity quickly disappeared after resting. Usually, the discomfort happens to happen to the hip joint area, but in some cases, it extends to the hips or knees. The gait remains unchanged, and the leg movements remain intact. On the X-ray film, a specific change was noted: subchondral sclerosis.
- level 2. The pain became more severe, appeared after exertion, and spread to the entire thigh and groin. After fatigue, a slight limp may occur. Found the difficulty in abducting the legs. X-rays show a significant reduction in the distance between bones (50% or more reduction), deformation of the femoral head, and significant bone growth.
- 3 degrees. The pain becomes permanent, and walking without crutches becomes impossible. When moving, the patient is clearly inclined to the painful side, which further increases the load on the joint. The range of motion is reduced and the muscles of the legs and buttocks are atrophy. The affected limb is shortened. X-ray showed obvious joint deformities, changes in the contour of the femoral head, and a large number of osteophytes.
- 4 degrees. The pain became more intense and did not stop for a minute, and the patient lost the ability to move independently. X-rays show complete destruction of articular cartilage and signs of bone fusion (stiffness). At this stage, it is only possible to deal with this disease through surgery.
diagnosis
Orthopedic traumatologists are responsible for identifying symptoms and choosing treatment methods. To diagnose and determine the extent of the disease, he uses:
- Investigation: listen to the complaints of patients and identify risk factors (trauma, disease, genetics, etc. );
- Check: assess the degree of movement of the limbs and determine the area of greatest pain;
- X-ray: X-ray images can assess the condition of bones and cartilage, the size of joint space, the presence and location of bone growth; in order to see the necessary details more thoroughly, the study supplements CT (computed tomography);
- Laboratory diagnosis: general blood tests can allow you to identify signs of inflammatory processes, biochemistry-pay attention to some risk factors, such as uric acid levels
- MRI (Magnetic Resonance Imaging): It can evaluate not only the condition of bones and cartilage, but also soft tissues: bones, ligaments, muscles, joint capsules, etc. ;
- Puncture the joints.
If it is necessary to make a differential diagnosis with other diseases, and to evaluate the accompanying pathology, additional tests, instrumental examinations, and consultations with specialists in a narrow sense are prescribed.
Hip joint disease treatment
The treatment of hip joint disease depends on its stage and severity of symptoms. Pathology requires a comprehensive approach using various methods:
- medical treatement;
- Non-drug therapy (physical therapy, exercise therapy);
- Surgery;
- Lifestyle correction and diet.
medical treatement
The drugs used for hip joint disease are designed to:
- Eliminate pain syndrome;
- Restore or at least slow down the destruction of cartilage tissue;
- Improve blood supply and nutrition in affected areas;
- Treat the accompanying pathology.
Analgesics are used in the form of tablets, intramuscular and intraarticular injections, and topical agents: creams, ointments, patches. In the early stages of disease development, non-steroidal anti-inflammatory drugs are sufficient for most patients. For severe pain syndromes, hormonal drugs are used. The analgesic is directly introduced into the joint capsule, and the effect is very good.
If the course of the disease is accompanied by muscle cramps, muscle relaxants are used. They are used in combination with other analgesics.
The time and dosage of analgesics should be limited to avoid further damage to the cartilage tissue and other side effects (especially the development of gastritis and gastric ulcer).
Chondroprotectants are drugs that help restore cartilage tissue. They are only effective if they are used regularly for a long time, combined with other treatments, lifestyle and diet adjustments. Drugs that improve blood microcirculation help enhance its effect. For a similar purpose, a warm ointment is prescribed. Only the doctor is involved in the choice of dosage and regimen.
Non-toxic treatment
This category includes various physiotherapy and manual techniques, as well as physiotherapy exercises. They help improve microcirculation and restore movement of damaged joints. Depending on the situation, the doctor will prescribe:
- Shock wave therapy
- Magnetic therapy;
- Electrical muscle stimulation;
- Various types of electrophoresis and ultrasonic electrophoresis (with the administration of anesthetics);
- Mechanical therapy
- Massage and exercise therapy.
Surgery
If the disease progresses to stage 3-4, medication and physical therapy will only relieve the patient's condition, but will not restore him to full mobility. In this case, arthroplasty is required, that is, a titanium prosthesis is used to completely or partially replace the damaged joint.
If there are indications, perform a lighter intervention: grind the contact areas of the bones and cover them with special smooth implants that facilitate sliding.
prevention
Lifestyle can significantly reduce the risk of hip joint disease and its progression rate. It is important to strictly follow the rules:
- Live an active lifestyle: swimming, walking, cycling in the swimming pool-amateur sports activities that do not participate in competitions help to improve blood supply and inhibit the process of joint degeneration;
- Normalize the weight to reduce the load on the legs;
- Eliminate injuries, hypothermia and occupational risk factors (vibration, weight lifting, standing work);
- Treat all diseases in a timely manner, including those that are not directly related to the musculoskeletal system;
- Correct postural obstacles in time and wear comfortable shoes.
diet
With the help of nutritional correction, patients can not only lose weight, but also reduce inflammation, salt deposition in tissues and metabolic disorders. It is recommended that you stick to a balanced menu that contains enough but not excessive carbohydrates, protein and fat, as well as vitamins and minerals. Special attention should be paid to unsaturated fats (olive oil and linseed oil), omega-3 acids (excess in fish), collagen (aspic, aspic). It is recommended to minimize fast carbohydrates, alcohol, espresso, products containing artificial flavors, preservatives and flavor enhancers.
Consequences and complications
Hip joint disease is one of the common causes of disability in the elderly. Without proper treatment, pathology will inevitably lead to complete disability, especially bilateral lesions. Pain and inconvenience prevent you from working and taking care of yourself, which is why it is important to receive treatment on time.













































